Sometimes, a person can experience one singular bout with a mental health disorder and never experience another. This is sometimes the case with clinical depression; after the initial episode, some patients find that they never again experience another depressive episode. Unfortunately, this is never the case with a person who suffers from Schizophrenia, a chronic mental illness that requires constant management from the moment of diagnosis onward. And while Schizophrenia affects approximately 3.5 million Americans at any given time, this disease is often misunderstood, leading to a systematic and widespread stigmatization of the Schizophrenic population that we must put an end to.
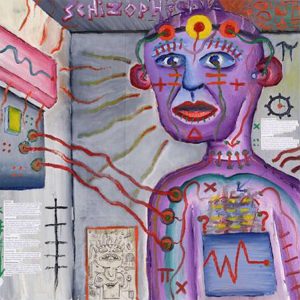
Let’s start by discussing what, exactly, Schizophrenia is. Schizophrenia is a brain disorder that distorts a person’s thoughts, ability to differentiate between fantasy and reality, and ability to relate to others. The DSM-5 Schizophrenia Spectrum Disorder classifies the following five key symptoms as indicators of this illness: delusions, hallucinations, disorganized speech, disorganized or catatonic behavior, and negative symptoms. To be diagnosed definitely with Schizophrenia, a person must experience at least two of these five symptoms with at least one of those symptoms matching the first three symptoms on the list (delusions, hallucinations or disorganized speech). Essentially, someone who suffers from schizophrenia is actually suffering from a dual diagnosis of both a mood disorder and psychosis, which, as you can imagine, can severely impact one’s ability to function and live a happy life without proper treatment and management. Left unchecked, schizophrenia destroys a person’s ability to differentiate between thought, behavior, and emotion, leading to an overall sense of mental disruption, a loss of touch with reality, and paranoia due to fantastical or delusional thoughts. And while you may think you’ve never met someone with schizophrenia, according to SARDAA (Schizophrenia and Related Disorders Alliance of America), it is estimated that between 1/3 and 1/2 of all homeless adults suffer from this disease, and a full 50% of people who have been diagnosed with schizophrenia have received no subsequent treatment post-diagnosis.
This is particularly alarming information when you consider that there is a very strong genetic component to this mental illness, which makes it that much more important for anyone who may be suffering from it to receive an official diagnosis, both for his sake and for his family’s. Furthermore, unlike other mental illnesses, schizophrenia does not present itself until late adolescence or early adulthood (SARDAA states that 3/4 of the schizophrenic population develops the illness between the ages of 16 and 25 years of age). The disease typically appears in the form of a change in behavior marked by the following symptoms, which must last for a minimum of 6 months straight: delusions (or strange beliefs that the person refuses to give up, even when provided with facts that contradict these beliefs), hallucinations (hearing, seeing or believing things that are not real), disorganized or fragmented thinking, odd or unusual behavior, slow movements or not moving at all, a lack of emotion in facial/physical expression and speech, poor motivation, and problems with speech and communication.
If you or a loved one has displayed these symptoms, it is absolutely imperative that they are first examined by a general practitioner, to rule out physical causes for this behavior. Then, if no physical explanation is identified, they must be seen by a mental health professional (ideally a psychiatrist with the power to prescribe and manage medication), who will use specific assessment tools and targeted questions to evaluate whether or not a diagnosis of schizophrenia is appropriate. Once an official diagnosis has been made, a plan of action can be laid out for managing their illness. This will most often be comprised of a combination of medication (often an antipsychotic drug taken in conjunction with a mood stabilizer), psychotherapy (to learn how to manage symptoms, set goals and gain insight into one’s own behavioral patterns), and skills training (special training in areas of difficulty, including work and social skills, self-care, and home and money management). In extreme cases, where the patient is at risk for hurting himself or someone else, hospitalization may be required until this risk is eliminated.
Although receiving a diagnosis of schizophrenia can seem like the end of the world, it is important to realize that it is much easier to fight a battle if you know what you’re fighting against. In closing, it is fully possible for a person with schizophrenia to live a full, happy, and productive life as long as they diligently manage their illness and moods and have a strong support system in place to lean on.